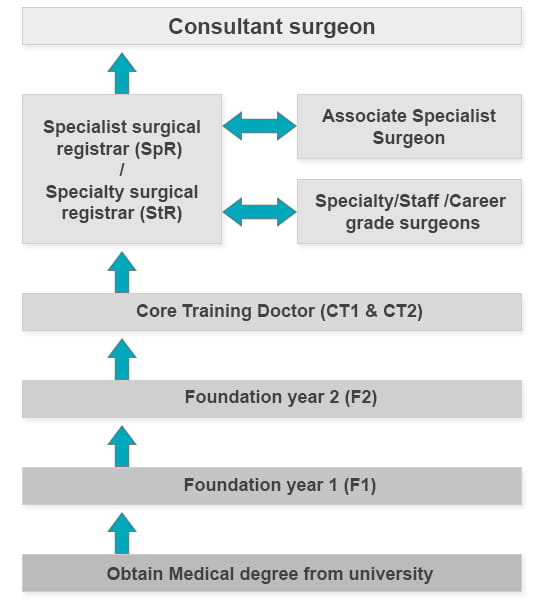
Who's Who in the Surgical Team
The surgical team consists of doctors with different levels of training, experience and responsibility, working alongside other healthcare professionals with different roles and responsibilities.
Consultant surgeon
The consultant is responsible for managing your care and is assisted by a team of doctors and other professionals. While you may see your consultant at hospital appointments and on the ward, s/he may not perform your operation. The consultant has overall responsibility for the standards of care given to all patients by doctors in their team. Consultants usually specialise and may become highly skilled in one or two specific areas of surgery. In order to become consultants in the NHS, their names must be on the specialist register of the GMC. In teaching hospitals, consultants may be called professors, readers or senior lecturers. Consultant surgeons employed by a university who have a contract with a hospital may be called honorary consultants.
Associate specialist surgeons
These surgeons carry out a wide range of surgical care, dependent on the extent of their training on the ward, in the outpatient clinic and in the operating theatre. This might include complex surgery at which they have become expert. They work under the supervision of a consultant. They too will often run their own clinics, have their own personal waiting lists and operate independently.
Specialty/staff grade/career grade surgeons
These surgeons will have had some experience as a registrar (see below) and have completed at least two years of surgical training after their foundation years (except specialty surgeons, who may have just finished core training). They may perform a range of operations and outpatient consultations under the supervision of a consultant. Depending on experience, career grade doctors tend to focus on a few specific routine operations. They will often run their own clinics, have their own personal waiting lists and operate independently. Some career grade doctors will also have teaching responsibility.
Specialist surgical registrar (SpR)
Before 2007 surgeons who wished to build up their surgical experience would apply for these posts, which typically lasted for six years. As a result, there remain a few of these surgical SpRs in post. As with StRs, they have to pass further exams, after which they become FRCS. After their training and examinations are successfully completed they can be awarded the CCT and, as per the above, become eligible to apply for positions as consultants. In teaching hospitals, an SpR may be called a research registrar.
Specialty surgical registrar (StR)
Doctors at this grade will usually spend six to eight years at this level building up experience. After the two years (sometimes less) of core surgical training across different areas of surgery, doctors can sit the MRCS (Member of The Royal College of Surgeons) exams. This, along with other assessments, enables them to continue their training. They then revert to the title Mr, Mrs, Miss or Ms, instead of Dr. This is due to tradition; in the past surgeons did not have to complete full medical training and so were not allowed to be called doctor. After a further four to six years of training and passing further exams, they can become FRCS (Fellows of the Royal College of Surgeons). On successful completion of this training period, surgical StRs are awarded the Certificate of Completion of Training (CCT), thus gaining entry to the specialist register and can apply for positions as consultants. In teaching hospitals, an StR may be called a research registrar.
Core training doctor (CT1 and CT2)
Following the completion of F2, core surgical training posts are where the surgeon gains experience performing different surgical procedures. Core training programmes will last up to two years (CT1 and CT2) depending on the grade and specialty. Doctors in these posts were formerly called junior surgical trainees.
Foundation doctors (F1 and F2)
All newly qualified doctors spend two years in training as foundation doctors. At least three months must be spent in surgery and three months in general medicine. Foundation doctors will typically spend four months on a placement. Once they have completed their first year of training, they are eligible for full registration with the General Medical Council (GMC). On surgical teams, foundation doctors are mainly concerned with preparing patients and observing procedures conducted by the surgical trainees. Foundation doctors with a keen interest in surgery may be given opportunities to assist in minor elements of surgery under close supervision.
Other healthcare professionals involved in surgery
Anaesthetists
On the completion of seven to eight years of specialist training, the GMC award a CCT which allows the holder to apply for a consultant anaesthetist position. More information can be found on the Royal College of Anaesthetists website.
Theatre nurses
Theatre nurses work with patients of all ages and primarily within hospital operating theatres and anaesthetic/recovery areas. Registered nurses are able to take on this role following specialist training and are regulated by the Nursing and Midwifery Council.
Operating department practitioner (ODP)
ODPs are a vital part of the clinical team and provide professional expertise during the patient's stay in hospital. Although they are primarily employed within operating theatres, they are increasingly being recognised for their skills in other critical care areas. Training will generally be two years in a higher education institution, once qualified, ODPs are regulated by the Health and Care Professions Council.
Surgical assistants/surgical care practitioners
Surgical care practitioners (SCPs) are non-medical practitioners such as nurses, operating department practitioners or physiotherapists who have extended the scope of their training to work as members of surgical teams. They can perform surgical interventions and preoperative and postoperative care under the supervision and direction of a consultant, although not independently. SCPs’ tasks include carrying out work in clinics, conducting pre-operative assessment and facilitating the continuity of patient care on the wards. They undergo a two-year part-time clinically based course at a higher education institution. The SCP curriculum, which was originally published in 2006, has recently been updated.
Visit our pages about the SCP curriculum for more information.
Podiatrists
Podiatrists have not completed a medical degree, but have instead trained exclusively in the surgical and non-surgical treatment of the foot, undertaking an honours degree in podiatry. They are regulated by the Health and Care Professions Council.
